Table of ContentsClose

Bipolar disorder remains a vexing problem. The illness affects approximately 5.7 million American adults—nearly 3% of the adult population, according to the National Institute of Mental Health.
Researchers estimate that between 25% and 60% of people with bipolar disorder attempt suicide at least once in their lifetimes, and between 4% and 19% die by suicide. Bipolar disorder also cuts an average of 9.2 years off a person’s lifespan, and not just by suicide. Patients with bipolar disorder are also more likely to have depression and develop conditions like arterial atherosclerosis and heart failure.
Despite the pressing need to help these patients, the condition is not widely understood, and effective medical treatments are limited. Lithium remains the most effective treatment but has side effects—tremors, weight gain, impaired memory and concentration, and muscle weakness, among others—that often prompt patients to discontinue use.
The Bipolar Disorder Research Program of Excellence, which is housed within the Iowa Neuroscience Institute at the University of Iowa, aims to change that. Iowa researchers are taking a multidisciplinary approach to better understanding bipolar disorder with the hope of developing new diagnostic markers and treatments to help patients.
“We’re trying to understand what’s happening in the brain for patients with bipolar disorder more comprehensively,” says Vincent Magnotta (94MS, 97PhD), professor of radiology in the University of Iowa Carver College of Medicine and co-lead investigator of the research program.
Much of the team’s work centers on one key finding made by Iowa researchers: Patients with bipolar disorder have abnormally acidic pH levels in the cerebellum, which is a section of the brain located at the back of the head that plays a major role in motor control.
“We wanted to know the significance, causes, and potential implications of this changed pH, which ended up being just the start toward really exploring ways that we can better understand bipolar,” says John Wemmie (96MD, 96PhD, 00R), professor of psychiatry and leader of the Bipolar Disorder Research Program of Excellence.
That discovery has grown into a program that now includes 12 faculty, 52 trainees, and 30 grants worth more than $28 million in funding. Together, these researchers are tackling the problem from four different approaches.

Learn more about the four different approaches
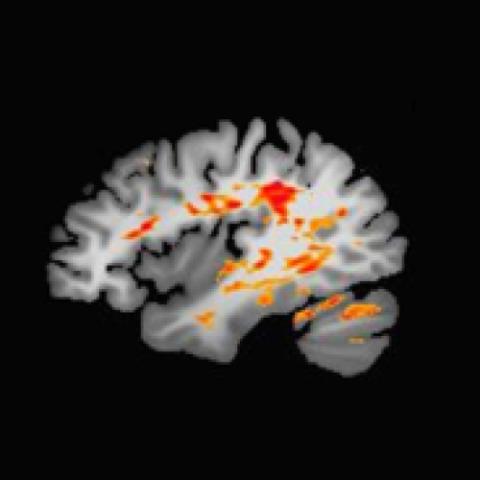
Brain imaging
Conducting brain imaging on the same research participants over time and at different stages of their illness is helping Iowa researchers better understand the nuances of bipolar disorder.
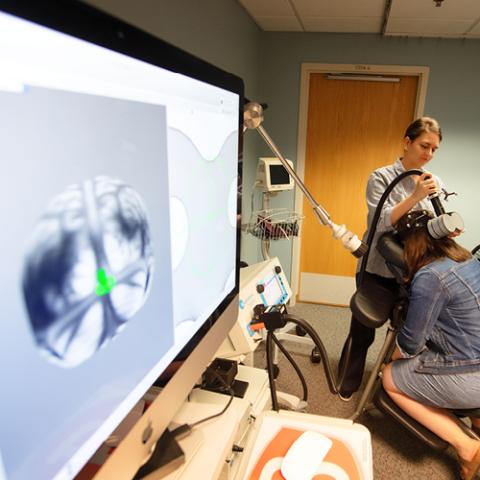
Cerebellum-targeted TMS
Researchers are still in the discovery phase of using repetitive transcranial magnetic stimulation (rTMS) directly on the cerebellum as a novel treatment option for bipolar disorder.

Modeling a bipolar brain
Using electrophysiology, researchers are measuring brain activity and connectivity—in hopes of better understanding exactly how the cerebellum works, and to possibly reveal its role in bipolar disorder.
Stem cells and genetic approaches
An Iowa team is using patients’ skin cells to create stem cells, which are then turned into neurons. These neurons might offer insights into...
Brain imaging
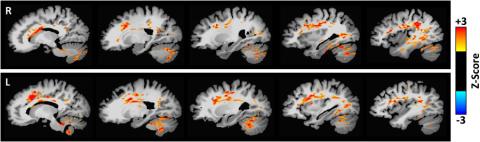
That means conducting imaging not only as they age but also at different parts of their mood spectrum, including when they are depressed and manic, Magnotta says.
Traditionally, that hasn’t been easy to do. But because Iowa has enrolled a group of 150 patients that they image repeatedly, it’s easier for researchers to work with them throughout the course of their illness.
“Studying patients serially over time and asking how they change from moment to moment is part of the process in discerning what these abnormalities are doing,” Wemmie says. “Are they a result of bipolar disorder, or a cause of bipolar disorder? Once we begin to answer those questions, we can start thinking about treatments.”
Cerebellum-targeted TMS
In these treatments, magnetic stimulation is applied directly to cerebellum—the same area of the brain that has a more acidic pH in patients with bipolar disorder.
“The magnetic field passes unimpeded through your skull to activate or inhibit areas of your brain,” Trapp says. “It’s easy to do and doesn’t have the same side effects of other kinds of brain stimulation or medication. We think it holds tremendous promise as a novel treatment approach to illnesses that have failed to respond to traditional pharmacologic and psychotherapeutic efforts.”
So far, the team’s studies have confirmed that cerebellum-targeted TMS is safe, and it is sufficient to change functional connectivity between the cerebellum and forebrain emotional control sites. This line of study is still in the discovery stage, however, and raises additional questions: Does it work? Does it need to be applied to a specific area of the cerebellum? Is the stimulation applied at the right time? Is it the right dose?
“It’s helping us calibrate treatments going forward and better understand how this treatment is interacting with the brain so we can develop better therapies down the road,” Trapp adds.
Modeling a bipolar brain
“When you’re trying to figure out how the brain works, you have to do your best to look at different phenotypes—or different behaviors that are abnormal with humans with bipolar disorder—and translate that to animals or induce it in some way,” says Krystal Parker, PhD, assistant professor of psychiatry, who has been working on this with John Freeman, PhD, professor of psychological and brain sciences.
Instead, researchers are using electrophysiology to measure brain activity in healthy animal models. They’re analyzing these patterns in hopes of better understanding exactly how the cerebellum works, and to possibly reveal its role in bipolar disorder.
So far, they have been able to record brain patterns from different regions of the brain at the same time. They’ve found that the cerebellum is critical for communicating contingency errors to forebrain sites involved in mood and cognition.
“The cerebellum doesn’t work by itself. It’s a network, so we’re really interested in not only how it works but also if it’s involved in different cognitive tasks, or if it’s interacting in other areas of the brain,” Parker says, adding that they’re also using this approach to see how drugs and rTMS affect the brain, as well.

Uncovering brain disorders
The Iowa Neuroscience Institute is fostering collaborations among researchers to find causes of— and the preventions, treatments, and cures for—the many diseases that affect the brain and nervous system.
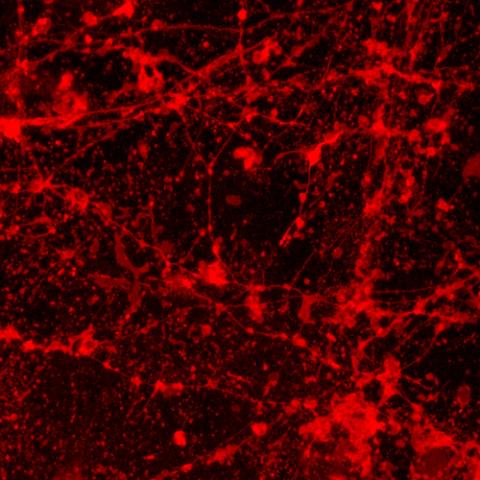
Stem cells and genetic approaches
“We found that individuals with bipolar disorder have different amounts of T-cells and monocytes than those without bipolar disorder,” she says, adding that these are markers of inflammation. “That could explain why these patients have a higher risk of developing comorbidities like heart disease, which itself is linked to immune changes.”
Gaine also hopes to find “a biomarker to tell what stage a person is at or if we can possibly treat symptoms of bipolar disorder by targeting these immune changes,” she says.
Aislinn Williams (10MD, 10PhD), assistant professor of psychiatry, is using patients’ skin cells to create stem cells, which are then turned into neurons that they can study, without patients undergoing major surgery. With those neurons, the team looks to see whether or not neurons of patients who have bipolar disorder express different sets of genes from those who don’t.
“We also look at how neurons develop over time because we have a hypothesis that people with bipolar disorder probably have something going on in their brain before they developed the condition that put them at risk for it,” Williams says.
This is key, because most people develop bipolar disorder as adults, and there is some data to suggest that neurons follow a different developmental trajectory, she adds.
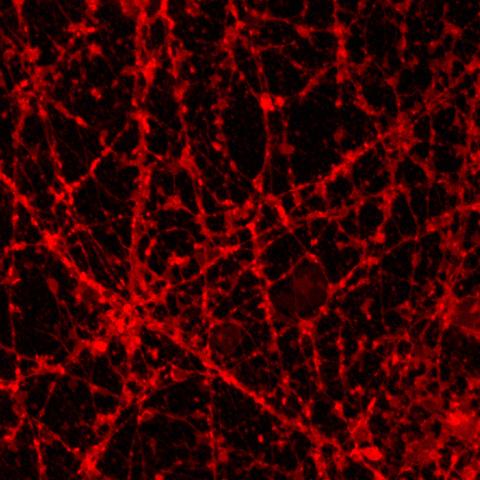
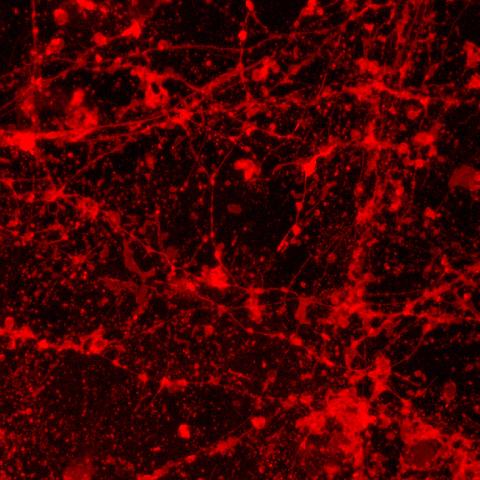
speckled appearance—compared to the control image. Neuronal beading is typically seen as a result of mitochondrial dysfunction which has previously been hypothesized in bipolar disorder. Images submitted by Karina Kruth, PhD, postdoctoral fellow.
Williams adds that none of this research would be possible without patients who are willing to participate in studies and treatment trials, whether that includes undergoing brain imaging during mania, or offering samples of their skin, blood, and DNA to researchers.
“They are magnanimous folks coming in for skin punch biopsies, which are not medically necessary, in order for me to create stem cells and do experiments that probably won’t benefit them,” she says. “They do it because they think it’s going to help somebody else.”
Despite these findings, bipolar disorder is still not well understood, but through this four-pronged approach to getting a better understanding of this disorder, Iowa hopes to advance knowledge of what is happening in these patients, potentially leading to new therapies and treatments.
“If we approach this from multiple angles, it really increases the rigor of the analysis and ability to discover the causes and underpinnings of what’s going on,” Wemmie says. “That will lead us to figure out what to do next.”
Top illustration by Bruce Hutton.
