Healing the healers
Gerry Clancy is addressing what he calls "pandemic-informed" burnout with a plan to help health care providers enjoy their work, feel fulfilled, and stay in the game.
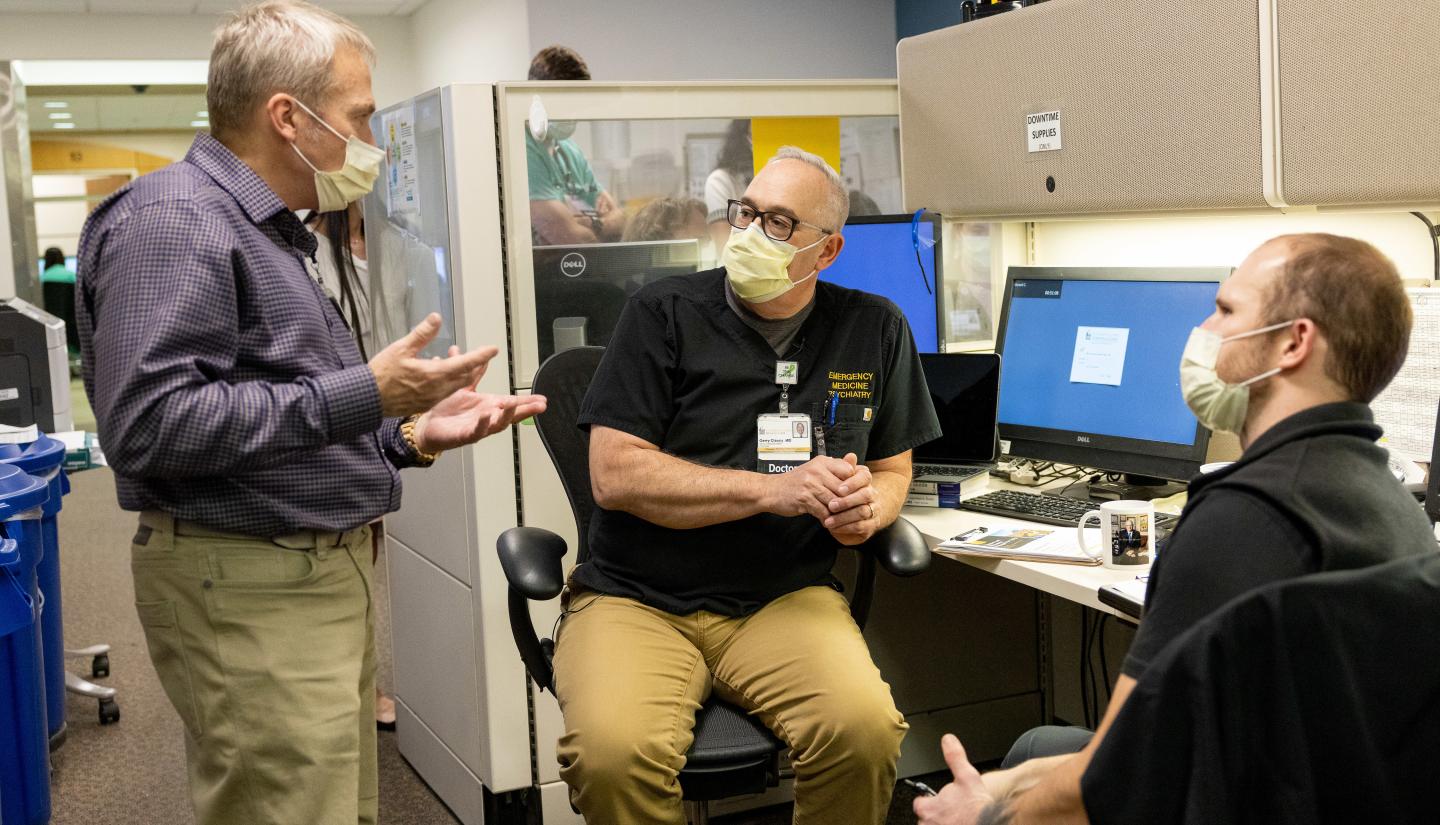
On an average day, Gerry Clancy (88MD, 92R) walks roughly seven miles to check in with physicians and staff on the front lines of patient care at University of Iowa Hospitals & Clinics.
These conversations have given him a clearer understanding of how the pandemic has changed health care providers’ mental and physical well-being.
“Medicine is the greatest profession,” says Clancy, who is the senior associate dean for external affairs in the Carver College of Medicine. “In this phase of my career, I’m trying to help existing health care professionals enjoy their work, feel fulfilled, and stay in the game.”
But for many health care providers and staff, staying in the game is increasingly challenging after a pandemic that has left much of the workforce exhausted. Medicine Iowa spoke with Clancy, who also serves as a professor in the college’s psychiatry and emergency medicine departments, about his enterprise-wide plan to prioritize clinician safety, well-being, and restoration.
Addressing physician well-being, restoration, and retention
Q: How do you define burnout in health care?
A: The old definition of burnout was just, "I'm exhausted and don't enjoy work anymore; I'm frustrated with all the technology; I've lost my self-determination." This new version of burnout is really pandemic-informed burnout. We need to truly understand that the pandemic was a huge threat to us. Do you remember Maslow’s hierarchy of needs theory from psychology?
If you look at what the pandemic did, it threatened our physiological needs. We were physically in danger. Our social needs were unmet because our social networks were blown apart. So, of course, we struggled with being able to really work at the top of our game because the foundational pieces of our security were very much threatened.
And the younger folks were affected so much more by the family and schooling issues than the older folks. The rates of burnout now are higher among our younger physicians than our older physicians—and we see the same with nurses and all other health care providers.
Q: When did you notice this shift to providers experiencing pandemic-informed burnout?
A: The big lightbulb moment for me was when the Delta variant hit in the fall of 2021. During the early part of the pandemic, people really pulled together. Even our internal messaging, “We're all in this together,” worked incredibly well. And, across society, you actually saw a decrease in suicide rates at the start of the pandemic.
But as the pandemic wore on, people started getting tired and really starting to struggle, including within our clinician group. And then Delta hit, and Delta was able to evade the vaccines and spread like wildfire. That’s when I saw the demoralization set in. At the time, some of our residency directors said, "Will you come and talk to us to get us through this?" And so, we started building peer-to-peer workshops around figuring out a way to just get through the next few months.
But then Omicron hit, and the general feeling went from demoralization to just exhaustion. And the staffing issues really started to kick in then. So, the workshops changed a little bit, and became much more about, ‘let's figure out, with the cards we are dealt with, how do we make the workplace work better?’
Over the course of the pandemic, I’ve now held 61 workshops throughout Iowa and trained about 3,000 health care professionals at the university and across the state.
Q: Why is promoting physician well-being a priority for you at this point in your career?
A: Medicine can and should be incredibly rewarding. And for me, helping the next generation of providers expands its impact. When you help a physician, you help a thousand patients. It's that ripple effect. But this pandemic was like a hurricane that blew through, and there's a lot of damage out there. And when we used to talk about burnout, there was a lot of focus on resilience. I will tell you; our nurses and doctors have been more than resilient. We do not have a resiliency issue with our nurses and doctors. They're tired, they're worn out, they're exhausted. But they are resilient. So, how do we bring them back up? Because the work can be incredibly rewarding. There’s a term called “post-traumatic growth,” which means that after really, really tough experiences, you can become wiser and stronger.
This is not to say the pandemic in any way was a good thing, but it was thrown at us and there are things we can learn from it. Maybe we can build a better health care system as a result. And the next time a threat comes like this, we'll be better prepared.

Q: Can you tell us more about your workforce well-being, restoration, and retention plan?
A: UI Health Care is taking a pyramid approach to addressing these needs. We are working really hard on workplace safety. I've done a fair number of workshops with our most at-risk departments on being able to identify when they're in a dangerous situation. We’re improving efforts to make this a safer environment in more than just physical ways. We’re improving access to physical and mental health care for our residents, expanding peer-to-peer mental health first aid training, and reducing the cost for various UI wellness programs and services.
We’re working on improving workflow. I’m pushing to make sure that we're not wasting time on things that aren't particularly fruitful. We do a lot of compliance trainings here in medicine. Can we make those more efficient?
And professional development is really important. We’ve established the THRIVE [Teaching, Health care, and Research Innovation through a Vibrant Environment] program and the “Rounding@Iowa” podcast to make it easier to get continuing medical education credits.
We want to make health care a better place to work, and we have to do it together. This work is piece after piece, after piece, after piece. But when it all comes together, it's a mosaic.

Listen to Rounding @ Iowa
This is the first episode of THRIVE@Carver, a special series on leadership in medicine.



