Table of ContentsClose
Cancer can't hide
Advancing immunotherapy for melanoma
Traditional cancer treatments fall into three categories: surgery, radiation, and chemotherapy. While these methods can be effective, they often come with their own serious side effects. Surgery can be disfiguring. Chemotherapy can be toxic to healthy cells. Radiation, particularly when used in treating childhood cancers, can lead to future health problems—including new cancers—sometimes years down the road.
Over the past two decades, however, immunotherapy has emerged as a fourth category of cancer treatment. It involves harnessing the body’s own immune system to mount a defense against abnormal cancer cells that have avoided detection. Immunologically speaking, most cancer cells, as they arise from normal tissues, are too much like the rest the body for the immune system to recognize them as “foreign” and be able to reject them.
Immunotherapy is a way to hang a hazard sign on a tumor in order to flag the immune system to take a closer look and respond accordingly. It is already working for some cancers—lung, kidney, and head and neck cancers as well as Hodgkin lymphoma and other cancer types—with fewer side effects than many treatments commonly used today. Additionally, immunotherapy can be effective against tumors that have resisted conventional treatments. It’s revolutionizing cancer care and could have an even greater impact in the years ahead.
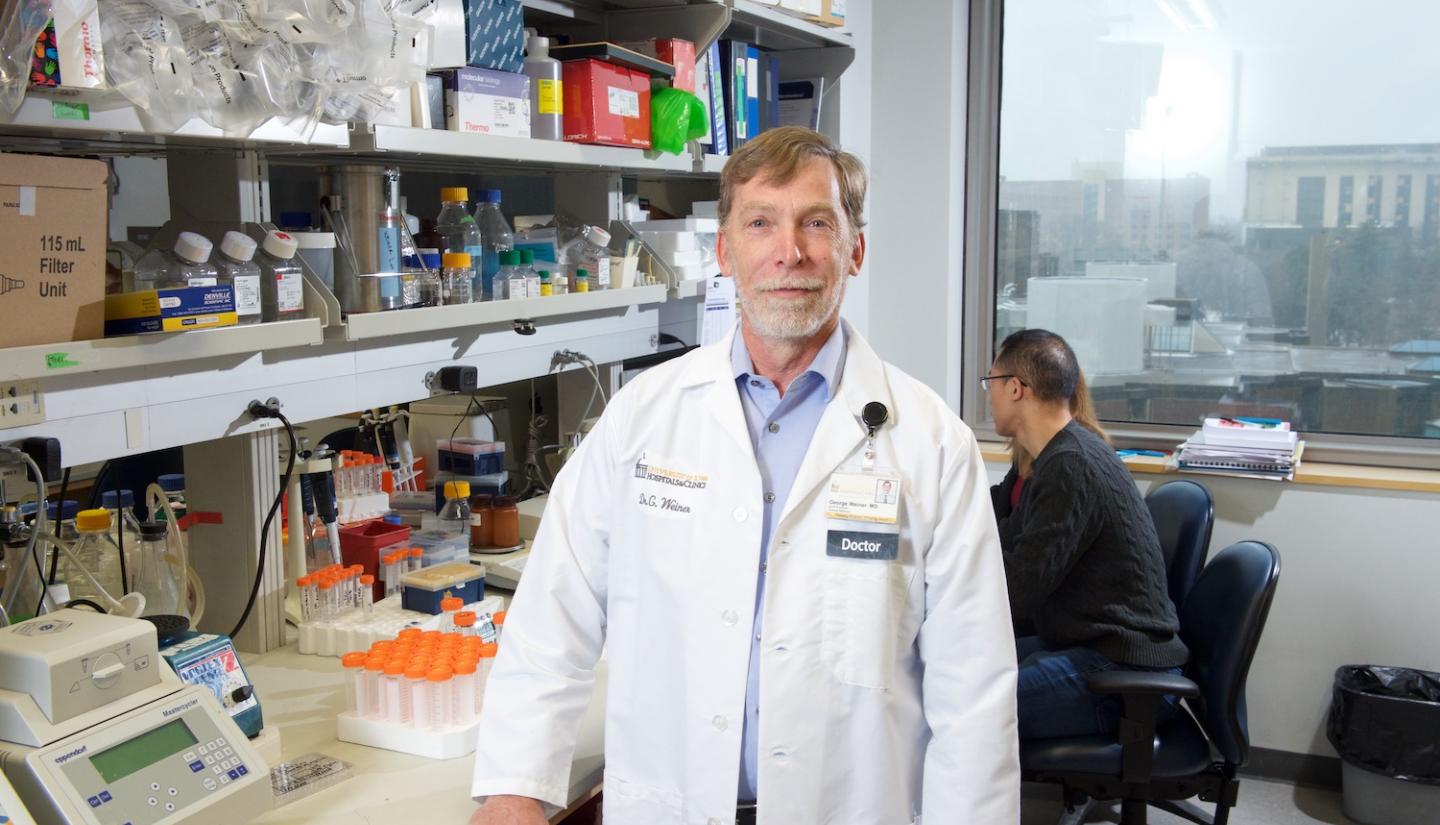
This is remarkable in that, until recently, relatively few cancer researchers and clinicians thought immunotherapy would succeed, notes George Weiner, MD, director of University of Iowa Holden Comprehensive Cancer Center.
Scientists had been trying to get the body to do this for more than a century, and when I started in the field, there hadn’t been a lot of evidence that it would work,” Weiner says. “But there were enough anecdotal reports about a handful of patients where immunotherapy worked extraordinarily well that many researchers continued to pursue the potential of inducing immune rejection of cancers. This persistence has paid off. We are finally starting to figure out how to make it work for more patients.”
Years of research have led to greater understanding of how cancers are able to hide from the immune system. Hence, the newest generation of immunotherapies work to not only stimulate the immune system but also inhibit the cellular checkpoints that prevent the immune system from recognizing and attacking cancer cells.
While immunotherapy has proven to be effective across a range of cancer types, it doesn’t work for every patient. For example, the use of anti-PD-1 (a checkpoint module) monoclonal antibodies, which were first approved by the Food and Drug Administration in 2017, has helped in triggering a patient’s natural immune system to fight melanoma and several other cancers. But it still doesn’t help all the seriously sick patients who need it.
In one nationwide, multicenter phase 1 study led by Holden researchers, nearly 25% of patients who have no other good options for their cancers are responding to immunotherapy treatment.
Holden Comprehensive Cancer Center researchers are currently testing another immunotherapy treatment option for melanoma based on CpG oligodeoxynucleotides (CpG ODNs), which are short, synthetic strands of DNA. Iowa researchers have been working on this specific form of cancer immunotherapy for decades. The drug CMP-001, which contains a CpG ODN and activates tumor-specific immune system responses, is now in multiple clinical trials and showing promising results. In one nationwide, multicenter phase 1 study led by Holden researchers, nearly 25% of patients who have no other good options for their cancers are responding to treatment.

Along with Checkmate Pharmaceuticals Inc.—a Cambridge, Massachusetts-based company founded by former UI Carver College of Medicine faculty member Arthur Krieg, MD—Holden researchers are continuing to explore CMP-001 as a new option for cancer patients.
"It’s something sorely needed for patients who are not treatable right now," says Mohammed Milhem, MBBS, associate director for clinical research at Holden. "It’s an oasis in a desert and important in us figuring out how to potentially target the immune system to work."
Research lines converge
The path to the Checkmate Pharmaceuticals’ CMP-001 showing progress in melanoma started more than 30 years ago, when Krieg and colleagues noticed something odd in a rheumatology study and thought it could be applied to cancer care: Instead of stimulating the immune system in harmful ways against itself, it could be prompted to attack tumors instead.
Krieg was doing research in rheumatology when he and Weiner joined the UI Department of Internal Medicine in 1989. While the crossover into cancer research may not seem obvious, rheumatological diseases, like rheumatoid arthritis and lupus, are often the result of an overactive immune system prompting the body to attack itself. Additionally, chronic inflammatory diseases can predispose these patients to a greater risk of cancers later in life.
As part of the research, “Dr. Krieg found, quite by accident, that certain short sequences of DNA were stimulating parts of the immune system,” says Weiner.
That finding was CpG ODNs. The Iowa researchers determined that these sequences are similar to those found naturally in bacteria and viruses and can prompt immune system cells, including B-cells (a type of lymphocyte, or white blood cell), into action.
Instead of tossing out the results as a fluke or as not useful to rheumatology, Krieg reached out to cancer immunologists, including Weiner, to see if these DNA sequences could be used to treat cancer.
“Dr. Krieg had a hypothesis that autoimmunity in humans was caused by endogenous retroviruses,” says Gail Bishop, PhD, professor of microbiology and immunology in the UI Carver College of Medicine. “He wasn’t finding convincing evidence to support that, but then he had this odd finding.”
Bishop’s research expertise includes B-cells, which are an essential part of the innate immune system that respond to viruses and bacteria that shouldn’t be in the body. B-cells make antibodies against invaders, and it appeared that CpG ODNs derived from bacterial DNA prompted these B-cells into action. The team, which included Weiner, Krieg, and Bishop, published its first paper on the finding in Nature in 1995.

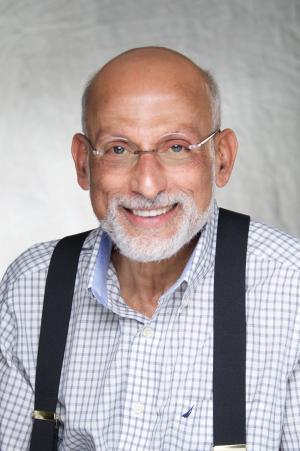
A decade earlier, immunologist Zuhair Ballas, MD, professor of internal medicine in the UI Carver College of Medicine, had shown that a certain subset of lymphocytes known as natural killer (NK) cells can, upon activation in vitro, differentiate into “super killers” that could eradicate a number of tumors.
Ballas reached out to Krieg to see if CpG ODN could activate NK cells. They found that some of these CpG ODNs were extremely effective in doing so. In a mouse model, Ballas showed that some CpG ODNs induced complete regression of melanoma tumors.
“It was the convergence of two lines of research,” Ballas says.
The initial cancer studies with CpG at Iowa involved patients with lymphoma, which was the focus of Weiner’s research. This work continues to this day.
“Melanoma came later, partly because we saw that CpG could activate natural killer (NK) cells that we know are important in the immune response to melanoma,” Weiner says.
NK cells are the first line of the innate immune system’s response against cancer. In melanoma, however, that response can be suppressed, thereby allowing the cancer to grow unchecked. Thus, if those NK cells could be prompted back into action by Toll-like receptors—specifically, TLR9—it could become a melanoma treatment.
“It’s a way for the immune system to detect that there may be a bacterial or viral infection going on. What we do is convince the immune system that something bad is going on in the cancer,” Weiner says. “The immune system rushes in, thinking it’s going to find an infection, but what it finds is the cancer. This can stimulate the immune system to fight the cancer.”
Iowa leads melanoma clinical trial
CMP-001, a TLR9 agonist containing CpG being developed by Checkmate Pharmaceuticals, underwent multiple pre-clinical studies, including through the Lymphoma Specialized Program of Research Excellence (SPORE) at Iowa, before entering clinical trials.
Milhem and his Holden colleagues are leading a nationwide phase 1B clinical trial on CMP-001 in melanoma. Patients are given CMP-001—injected directly into tumors—plus an anti-PD-1 monoclonal antibody, or they’re given a CMP-001 injection only.
Early findings, presented by Milhem at the Society for Immunotherapy of Cancer annual meeting in November 2020, are promising. Out of 98 patients treated with CMP-001 plus anti-PD-1, lesions in seven had complete responses—that is, lesions disappeared to the point they could not be seen on any kinds of medical imaging or scans—and 16 had partial responses, with responses lasting a median of 19.9 months. The most common treatment-related side effects were flu-like symptoms and injection site reactions.
Milhem says that while these results are preliminary, “It’s a very strong signal that it’s working.”
The trial is set to run through May 2021 and will likely be followed by a phase 2 trial to “really hammer out what is the efficacy and what is the true response,” says Milhem. He notes that patients who enroll in these trials will play a key role in making it happen.
“They’re the heroes that really move the science needle to the point where we can see this going on to be something that gets FDA-approved and has the potential to help millions,” he says.

'We still have a lot to learn'
Despite the successes of cancer immunotherapy, the work is just beginning. CMP-001 alone and in combination with anti-PD-1 has shown to be effective in about 25% of patients with metastatic or unresectable melanoma that progressed on prior therapy that included an anti-PD-1 antibody. This leaves 75% of these patients for whom it does not appear to be effective. Studies with other types of cancer are just beginning, and researchers don’t yet know how patients with these other types of cancer might benefit from this new approach to cancer therapy.
“We still have a lot to learn about the details of how it works, how to use it, which patients might benefit, how to give it and in what combination, and how to deal with the side effects,” Weiner says. “When it comes to proving that this treatment is going to be effective for cancer therapy, it’s like having a lead at the end of the first quarter. It’s promising, but we still have a long way to go.”
University of Iowa Holden Comprehensive Cancer Center
Years of research have led to a greater understanding of how cancers hide from the immune system—and a promising immunotherapy treatment for melanoma.
