Table of ContentsClose

Advanced electrophysiology procedures and techniques at Iowa offer new options for patients with heart rhythm disorders.
When Keeli Frerichs arrived at University of Iowa Heart and Vascular Center with a perilously low heart rate, the collegiate soccer star just wanted to get back on the playing field.
But to cardiac electrophysiologist Paari Dominic, MBBS, MPH (12F), the young athlete represented more than another case of arrhythmia—she epitomized a movement.
The first-ever cardioneuroablation in the U.S. was performed in 2019.
Treated successfully in spring 2023, Frerichs became one of the first people in Iowa to benefit from cardioneuroablation, an intricate new procedure to treat dangerously low heart rhythm or fainting due to low blood pressure (vasovagal syncope). And Dominic, the medical director of UI Health Care’s electrophysiology lab, was uniquely qualified to help.
Returning to Iowa in January 2023 after eight years at Louisiana State University Health Sciences Center, he's among only a handful of electrophysiologists nationwide—and the only one in Iowa—who performs cardioneuroablation, which burns select nerve endings inside the heart to increase resting heart rate.
The technique signifies a vast improvement over medications and pacemaker placement—approaches traditionally used to treat patients like Frerichs. Cardioneuroablation is part of a wave of new treatments targeting the heart’s electrical system that have transformed UI Heart and Vascular Center into a destination hub for arrhythmia care.
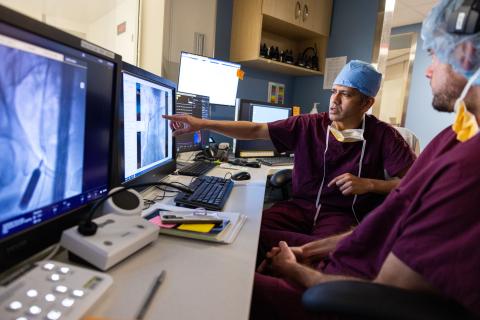
Performing 150 to 200 procedures each month, Dominic and his team—expected to grow to nine electrophysiologists and four nurse practitioners in 2024—have brought new capabilities to make these procedures safer and more precise. The team is building on an already-strong electrophysiology technology foundation; former UI electrophysiology fellow Shlomo Ben-Haim, MD (93F), is credited as a pioneer in developing new and enhanced techniques to precisely map electrical activity in the heart and identify the source of arrhythmias.
“I have an extremely cohesive group of faculty who work together, not only in improving patient care and efficacy but also in innovating newer procedures and techniques,” says Dominic, an associate professor of cardiovascular medicine in the Carver College of Medicine Department of Internal Medicine. “I feel we’re following in the footsteps of people before us and adding to their work.”

A breakthrough for central sleep apnea
UI Heart and Vascular Center provides more diagnostic and treatment options for arrhythmias than any other health system in Iowa, offering help for patients with irregular heart rates who haven’t found relief elsewhere. The team’s efforts are boosted by the addition of two new cardiac catheterization labs in the last two years, where nearly 4,600 minimally invasive procedures are performed each year.
One of these is the Remedē (pronounced “remedy”) system, available in Iowa only at UI Heart and Vascular Center. This new option treats moderate to severe central sleep apnea, which occurs when the brain doesn’t send proper signals to muscles that control breathing. Implanted in the upper chest, Remedē monitors patients’ respiratory signals during sleep and stimulates the phrenic nerve—responsible for breathing—to move the diaphragm if breathing becomes irregular.
Unlike obstructive sleep apnea, central sleep apnea is often the result of other conditions such as heart failure or stroke—preventing the brain from sending the correct signals to the muscles that control breathing. It’s a serious condition that can cause sudden death, and it’s one for which standard sleep apnea treatments such as continuous positive airway pressure (CPAP) typically are not recommended or effective.
Central sleep apnea patients “didn’t have an option before, especially when they had coexisting heart failure,” Dominic says. “That’s where Remedē comes into play. The expertise to place a Remedē device is still limited to a few electrophysiologists around the country, since it takes a specific skillset. We have that.”
Refining AFib treatments
Dominic and his colleagues also offer several new minimally invasive treatments for atrial fibrillation (AFib) that doesn’t respond to other therapies. The most common heart arrhythmia, atrial fibrillation has long been treated with medications and ablation procedures that use either heat or cold to block abnormal electrical signals responsible for the irregular heartbeat.
But as treatments evolve, UI Health Care has quickly adopted ablation techniques that offer a more personalized approach to each patient’s specific case. Available in Iowa only at UI Heart and Vascular Center, these new AFib treatments include:
The convergent procedure
A hybrid approach that combines minimally invasive heart surgery and traditional catheter ablation. It requires close collaboration between cardiac electrophysiologists and cardiothoracic surgeons—specialists who regularly work together at Iowa.
Vein of Marshall ablation
Which places a catheter inside the small Vein of Marshall at the back of the heart and injects alcohol in it to eliminate atrial fibrillation. Electrophysiologists at UI Health Care have already performed more than 30 such procedures and expect to publish their results.
Ganglionated plexi ablation
Designed for patients with a slow heart rate or whose vagal nerve activity triggers atrial fibrillation. The technique can prevent the need for a pacemaker by ablating nerves outside the wall of the left atrium of the heart's left upper chamber. "The majority of AFib originates in the pulmonary veins—they’re the trigger in 70% of cases—but we were able to improve on traditional ablation with ganglionated plexi ablation in addition to isolating those pulmonary veins,” Dominic says. “When we did, outcomes significantly improved.”
A Leading Lab
UI Heart and Vascular Center is Iowa's leading electrophysiology lab, offering an array of advanced atrial fibrillation treatments. Visit the link below for more details, including information on clinical trials that aren't offered anywhere else in Iowa.
On the pulse
Other advanced arrhythmia treatments available at UI Health Care include leadless pacemakers, which don’t require wires to be threaded from the shoulder area to the heart. Since these wires, called leads, can later malfunction, become infected, or cause other dangerous complications, eliminating them can be safer for patients. UI Heart and Vascular Center is also home to the only cardiac electrophysiologists in the state who perform complex laser lead extraction procedures when complications occur.
“Because these leadless pacemakers don’t have a lot of hardware, we can put small capsules directly into the heart that have a battery life of 12 to 20 years,” Dominic explains.
Like the full array of new advances, leadless pacemakers are revolutionary for their ability to offer patients solutions that didn’t exist before, and additional developments are imminent.
“Every year we’re getting something new that adds to the understanding of disease processes,
or technologies and toolkits to treat cardiac arrhythmias,” Dominic says. “There are so many things in the pipeline I’m really looking forward to.”
Ultimately, Dominic hopes the electrophysiology program at Iowa can be a model for other centers.
“The team we have now has this one focus in mind: to make UI Health Care’s cardiac
electrophysiology lab the most sought-after place in the country,” he says.
Paari Dominic: Back at Iowa, improving lives, feeling the love
Read an in-depth Q&A.

New Iowa-developed ablation technology gets FDA approval
The Farapulse™ pulsed field ablation (PFA) system received FDA approval in January 2024. UIHealth Care cardiac electrophysiologists are the first in Iowa to begin using the system.
The technology was developed by Farapulse Inc., a UI startup founded by Steven Mickelsen,
MD (13F, 14F), assistant professor of internal medicine-cardiovascular medicine. As a fellow
physician and then a faculty member in the Abboud Cardiovascular Research Center at Iowa,
Mickelsen conceived and built the prototypes that eventually became the Farapulse system.
Boston Scientific Corp. acquired Farapulse Inc. in June 2021.
Standard cardiac ablation requires an electrophysiologist to route catheters through the veins
to the heart and apply extreme heat or cold to damage misfiring heart cells. The Farapulse
system uses electrical signals that isolate and ablate specific heart cells in a precise pattern,
resulting in a quicker and safer procedure.
