Table of ContentsClose
Eat less and eat better.
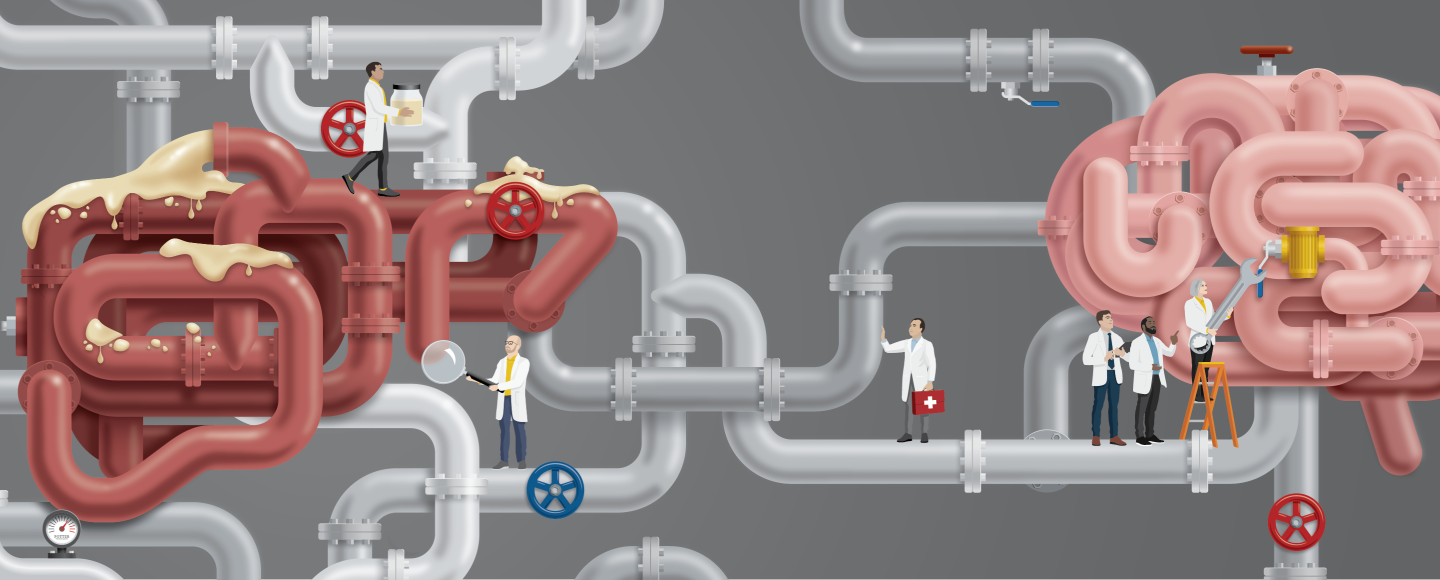
Advice for combating obesity and improving metabolic health is often delivered in these simplistic terms. While true, it misses the fact that our metabolic biology is incredibly complex, highly integrated, and easily disrupted by a modern food environment that has many of us consuming a diet too high in fat and sugar.
The biological effects of excess fat due to obesity increase the risk of a range of metabolic disorders such as heart disease, Type 2 diabetes, and steatotic liver disease, also known as fatty liver disease. These conditions cause chronic disease and death in millions of people worldwide.
Understanding the metabolic pathways that are involved in handling excess dietary fat — how they work, how they are interconnected, how we can intervene, and how some types of fat may be more toxic than others—may help researchers develop new therapies to improve metabolic health and reduce the health burden of metabolic diseases.
With studies that shed light on the biological mechanisms involved in fat metabolism and reveal new targets for treating metabolic diseases, University of Iowa researchers in the Fraternal Order of Eagle Diabetes Research Center are at the forefront of advancing this field. In just the past year, four UI-based teams have published their findings in Cell Metabolism, one of the top journals in the field.
“The breadth and quality of the research being done at the UI Fraternal Order of Eagles Diabetes Research Center is a testament to the collective strength of metabolic research at UI,” says Eric Taylor, PhD, professor of molecular physiology and biophysics in the UI Carver College of Medicine. “The work that we're doing here will have implications for millions of Americans who are affected by these diseases.”
Fat in the liver
The liver is a critical convergence point for metabolic pathways designed to manage and store excess fat. Calorie-rich diets can disrupt these pathways and cause fat to build up in liver tissue, leading to metabolic dysfunction-associated steatotic liver disease (MASLD).
MASLD is extremely common, affecting about one in three people. It is strongly associated with Type 2 diabetes, obesity, high blood pressure, and high cholesterol, and it is independently linked to an increased risk of heart disease and death. Left untreated, MASLD can progress to a more advanced form of fatty liver called MASH (metabolic dysfunction-associated steatohepatitis), which can lead to serious conditions like cirrhosis and liver cancer.
Reducing fat buildup in the liver is associated with improvements in MASLD, insulin sensitivity, and other markers of metabolic health. Thus, defining the pathways involved in liver fat metabolism could lead to new interventions to treat or prevent these conditions.
A study led by Taylor is one of the most comprehensive mappings of all the pathways involved in fat production in the liver. This normal physiologic process, called de novo lipogenesis (DNL), allows the body to convert excess energy into fat that can be stored for later use. However, elevated DNL contributes to MASLD, Type 2 diabetes, and increased risk of heart disease.
Because elevated DNL is linked to these health problems, drug companies are focused on making newer and better lipogenesis inhibitors. Current drugs are effective in blocking DNL, but they produce intolerable side effects — making them nonviable as therapies. The ability to improve treatment options has so far been limited by an incomplete understanding of all the metabolic pathways involved in DNL.
Taylor’s new study not only dissects known DNL pathways; it also identifies several new ones. The study shows that an enzyme called ACLY controls the major pathway mediating DNL. This is significant because bempedoic acid, a drug used for people with high cholesterol levels who can't take statins, targets ACLY. The finding suggests that bempedoic acid might also be useful for treating steatotic liver disease.
The study is also the first to genetically demonstrate the pathway for turning ketones into fat in the liver, and it’s the first to show that the amino acid leucine can also make fat through a direct ketogenic, lipogenic pathway.
“There are lots of different ways that the liver can make fat. To develop better treatments for fatty liver disease, we need to know how these ‘tributary’ pathways interact, what fuels they use, and what enzymes mediate them,” Taylor says.
Liver-brain axis
While Taylor’s study demonstrates the complexity of the fat metabolism pathways within the liver, two other UI-based research studies reveal previously unknown liver-brain connections that show how the brain plays a role in fatty liver, too.
Ling Yang, PhD, associate professor of anatomy and cell biology, discovered a brain-liver connection where obesity-induced cellular stress in the brain’s pituitary gland contributes to fatty liver disease.
Obesity is a state of abnormal circulating levels of pituitary hormones, which govern the body’s energy and metabolic homeostasis. Of note, the prevalence of obesity-associated metabolic diseases (such as steatotic liver disease) increases in patients with pituitary abnormalities. However, it is not known what the factors are that trigger the dysfunction of the pituitary gland in obesity.
Yang’s team examined a cellular mechanism known as the unfolded protein response (UPR) pathway, which protects cells from stress, in the pituitary glands of obese humans and mice. They found that obesity disrupts this stress response in the pituitary gland, impairing its ability to protect cells from stress caused by excess nutrients and inflammation. This pituitary cellular dysfunction, in turn, leads to abnormal pituitary hormone production and the resultant metabolic abnormalities in the liver by compromising the UPR in liver cells and disrupting their ability to handle cellular stress.
The findings also highlight the critical roles of hormones in connecting the cellular stress responses between the brain and the liver, showing that obesity-associated pituitary defects alter thyroid hormone levels, further exacerbating MASLD progression.
"Our study not only uncovers a previously unknown cellular stress response cross talk between the brain and the liver, but the findings may also have direct implications for strategies to treat obesity-associated metabolic diseases, including MASLD,” Yang says.
Indeed, the first U.S. Food and Drug Administration-approved drug for MASLD, resmetirom, is targeting the liver-thyroid hormone function.
UI researchers were also part of a study demonstrating another example of the emerging role of brain-liver connection in metabolic disease. This study shows that a molecule called FGF21 can reverse MASH through coordinated actions on the brain and the liver. Specifically, the researchers found that FGF21 acting on the central nervous system increases sympathetic nerve activity to the liver and reduces DNL. This lowers triglyceride levels in the liver and reverses a form of damage called fibrosis. The study shows that FGF21 can also act directly on the liver, reducing liver cholesterol levels. These results suggest that FGF21 might be a promising pharmacological target to treat MASH.
The research team was led by Matthew Potthoff, PhD, who was a professor at the UI and is now at the University of Oklahoma, and included Kamal Rahmouni, PhD, UI professor of neuroscience and pharmacology and interim co-director of the Fraternal Order of Eagles Diabetes Research Center.

Ceramides: the new cholesterol
The role of a different FGF molecule — FGF13 — is the subject of a fourth UI-led study, which focuses on ceramides. These are bioactive lipids, sometimes referred to as the “new cholesterol,” due to their ability to predict the onset of cardiovascular diseases. Ceramides are considered as one of the most toxic lipids, but they are important for regulating various metabolic processes.
Led by Bhagirath Chaurasia, PhD, UI assistant professor of internal medicine, this study finds that obesity, which increases ceramide accumulation in fat cells, promotes the production of FGF13. The increases in FGF13 levels damage the ability of fat cells to store and use energy, leading to impaired energy and glucose balance.
The findings identify FGF13 as a linchpin molecule in fat metabolism, translating the effect of increased ceramide levels into metabolic damage, and suggest that altering the activity of FGF13 might help to prevent and treat metabolic diseases.
"There has been a long-standing interest for drug companies to target ceramide synthetic pathway to improve metabolic health,” Chaurasia says. “However, due to the essential requirement of ceramides in key cellular processes, this has been challenging. The identification of FGF13 provides an alternative way to target this pathway and improve metabolic health without altering the ceramide levels.”
Finding new, better ways to treat metabolic diseases
As a leader of the Fraternal Order of Eagles Diabetes Research Center at the UI, Rahmouni notes the importance of these studies and other research involved in unraveling the biological pathways and whole-body systems that contribute to metabolic diseases.
“The goal of all the research and discoveries coming out of the UI Fraternal Order of Eagles Diabetes Research Center is to identify new and better ways to treat these incredibly common metabolic diseases and eventually improve the health and well-being of thousands of Iowans and millions of people around the world,” he says.
