Table of ContentsClose
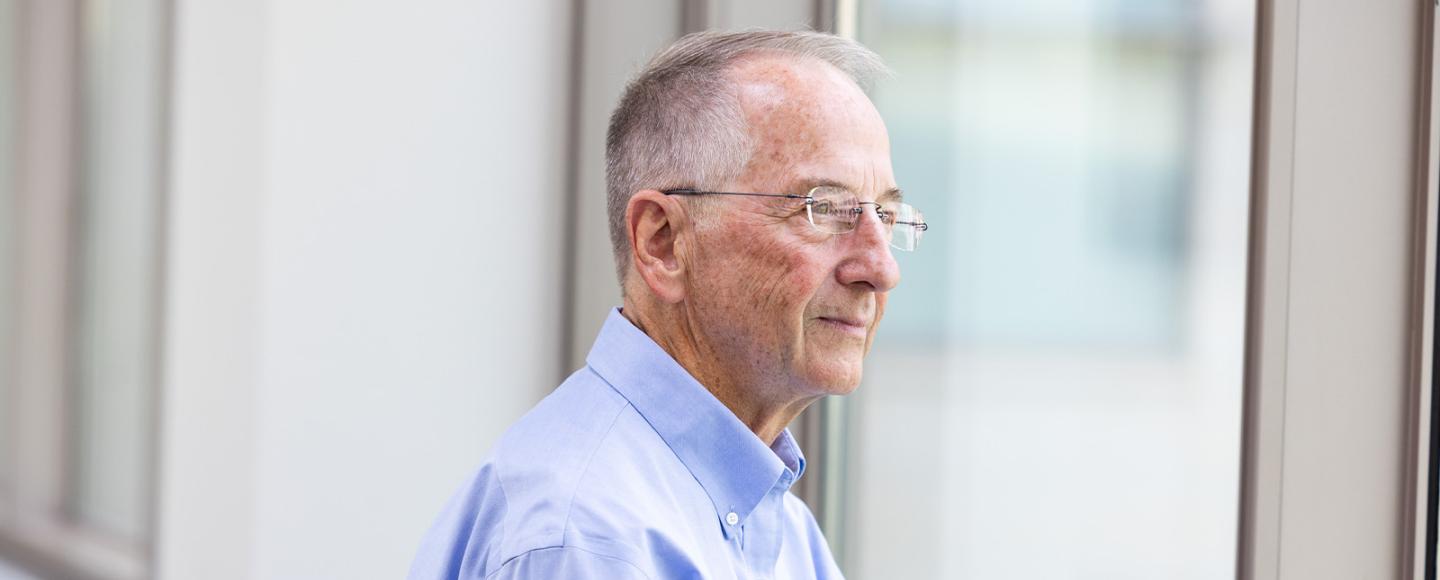
Over the course of a nearly 45-year career at the University of Iowa — and in collaboration with Carver College of Medicine colleagues and researchers at institutions around the nation and world — Michael Welsh (74MD, 77R) has helped lead a revolutionary improvement in the lives of individuals with cystic fibrosis.
By understanding and describing the cellular and molecular mechanisms behind this disease, Welsh’s research led to life-saving treatments that transformed cystic fibrosis from a terminal illness to a highly treatable condition for most patients.
These contributions have earned Welsh the 2025 Lasker-DeBakey Clinical Medical Research Award from the Lasker Foundation, which recognizes research discoveries that improved the lives of many thousands of people. Welsh shares the award with Paul A. Negulescu, PhD, of Vertex Pharmaceuticals and Jesús (Tito) González, PhD, formerly of Vertex, for their roles in developing a new treatment for cystic fibrosis.
The award follows other major international honors Welsh has garnered in recent years, highlighting how fundamental science, driven by curiosity and collaboration, can lead to life-changing innovations and therapies.
Meeting a young patient fuels a sense of purpose
Cystic fibrosis (CF) is a genetic disorder that damages the lungs, pancreas, and other organs, making it extremely difficult for patients with CF to breathe and get adequate nutrition.
As a medical student at Iowa in the 1970s, Welsh saw firsthand the devastating effects of CF in patients — notably, a young girl with a harsh, persistent cough who was forced to speak in brief sentences because she was constantly out of breath.
“I learned about all the things that she couldn't do because of her disease,” he says. “[When] I spoke with my attending physician, it was sobering because I learned that she probably was never going to make it to her teens. And if she did make it to her teens, she wasn't going to make it out of her teens.”
Welsh’s encounter with this girl is burned in his memory. It motivated him to find a way to impact the lives of patients with this disease.
Breath by Breath: Living with Cystic Fibrosis
See how research at Iowa changed our understanding of cystic fibrosis — and changed the lives of patients with CF.
A clearer understanding of cystic fibrosis
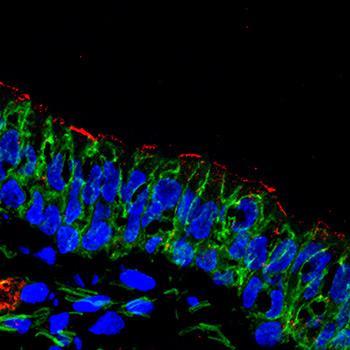
As a clinician and a biomedical scientist, Welsh was interested in how cells produce and maintain a thin, protective layer of mucus to capture and flush away bacteria and other irritants from the lungs, bronchi, and windpipe. In people with CF, this mucus is thick and sticky and clings to cells instead of “bathing” them—clogging airways and contributing to shortness of breath and frequent lung and sinus infections.
The thickened mucus from CF also affects the pancreas, blocking the flow of enzymes into the digestive tract. This, in turn, prevents the affected person from getting adequate nutrients from their food. This chronic problem in the lungs, pancreas, and other organs led to a very poor quality of life and was usually fatal.
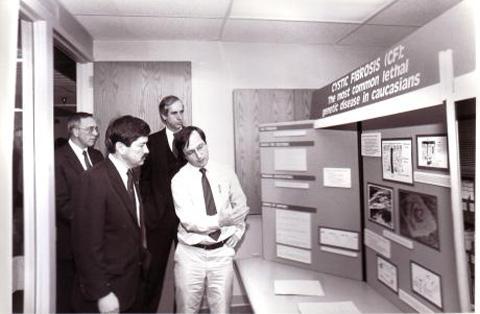
Welsh’s work on the biophysics of lung cells affected by CF demonstrated that chloride ions were not moving across the membranes properly. As his team continued their work on cellular dynamics, other researchers attacked the problem from a different angle. It had been clear that CF was an inherited condition, and in 1989, the then-emerging field of gene mapping achieved a breakthrough: Researchers at two other labs identified the gene responsible for CF, which became known as the cystic fibrosis transmembrane conductance regulator (CFTR) gene.
“Before the gene was discovered, we had a general idea about the workings of cells lining the bronchi and how they transport chloride,” Welsh says. “Then Lap-Chee Tsui at the University of Toronto and Francis Collins, then at the University of Michigan, discovered the gene that is mutated in people with CF. This knowledge set the stage to further study the gene and its product, the CFTR protein.”

Michael Welsh, MD
- Professor, Department of Internal Medicine–Pulmonary, Critical Care, and Occupational Medicine
- Professor, Department of Molecular Physiology and Biophysics and Department of Neurosurgery
- Director, Pappajohn Biomedical Institute
- Howard Hughes Medical Institute Investigator, 1989–2024
- Major Awards:
- 2018 Warren Alpert Prize
- 2022 Shaw Prize in Life Sciences and Medicine
- 2023 Wiley Prize in Biomedical Sciences
- 2025 Canada Gairdner International Award
- 2025 Yergin-New International Prize for Biomedical Research
- 2025 Lasker-DeBakey Clinical Medical Research Award

Iowa research leads to new CF therapies
Beginning in the early 1990s, Welsh and colleagues demonstrated that the CFTR protein is a channel that lets chloride flow through cell membranes. The researchers learned about ways that CFTR gene mutations disrupted its function. Over time, they discovered they could repair its function in the lab.
This deeper understanding enabled the classification of CF mutations and paved the way for targeted therapies to correct CFTR protein defects. Negulescu and González led the research team at Vertex that developed a new class of medications that specifically restore the protein’s function. One of these, Trikafta, is a triple-combination therapy with the potential to treat approximately 90% of patients.
As such, CF can be treated at the molecular level in ways that surpass past therapies that focused only on managing symptoms. Today, many patients with CF are living longer and with a significantly better quality of life.
‘No one does this alone’
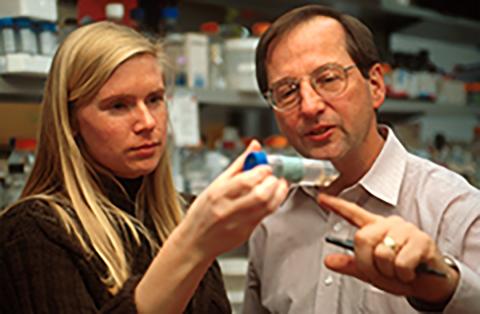
It’s difficult to estimate the number of patients Welsh has seen, students he has taught, and faculty, staff, and postdoctoral researchers he’s worked with over the years. But through it all, his profound curiosity and spirit of collaboration have been key. He unfailingly recognizes his research team and the essential part they’ve played throughout his career.
“I'm the beneficiary of fantastic students and fellows, and tremendous staff, colleagues, and collaborators. Because no one does this alone,” Welsh says. “It's incredibly important to surround yourself with people who are willing to challenge you, ask questions, and bring forth new ideas. It doesn’t matter whether someone’s a professor or a student. You have to encourage everyone to be critical and, importantly, to contribute, for that’s the way we make fundamental progress.”
Real impact
Three individuals with cystic fibrosis and taking the triple-combination therapy share their thoughts.

Cassandra Murphy, Davenport, Iowa
“It sounds really cliché, but when you grow up not knowing if you’re going to have an adulthood, it makes you appreciate things more ... I never thought in a million years I’d have a baby or get married. It’s awesome.”

Grace Lidgett, Traer, Iowa
“I’ve been off my [previous] treatments for a year and some now ... I’ve never felt more ‘normal.’ I get to live a life that everybody else lives.”

Jason Kielty, Coralville, Iowa
“I haven't been to the hospital in six years, and I was going every two-and-a-half to three months. It's been six years on Trikafta, and I haven't been back.”
Photos by Liz Martin
